Using Technology & Data For Mental Health
Our lofty goal is to half New Zealand’s suicide rate by 2025. You might think that’s not possible. Well, in fact, it is. New Zealand is currently ranked 53rd in suicide and for youth suicide, we’re ranked number one. It’s a shocking stat, showing we need a greater focus on mental health. But there are 47 other countries in the world that have a suicide rate that is half of New Zealand’s, so there is no reason why we can’t have a rate like Italy, or Mexico, or Greece. When we achieve that, we’ll be going for zero.
How are we going to do this? Well, one thing we are not going to do is more of the same. We simply can’t be doing more of the same, it doesn’t work. We’ve got to change things up, we’ve got to fix a broken model. If we keep doing more of the same, we’ll get the same results. We need to think about what we can do differently to better manage, assess and prevent mental health in this country.
The primary care medical model for mental health that we’ve always used is broken. It’s a commoditised sector, time for money. GPs charge a certain fee and they’ve got to get through a number of patients every day to pay the bills. So they have 6-10 minute consultation times. 6-10 minutes to ask you a whole bunch of questions around your mental health.
I’ll paint this picture: It’s 10am, the patient has finally built up the courage, five minutes into their 10 minute consult, and tells the doctor that their feeling depressed, they think their wife is going to leave them and they could lose their job. The doctor looks at their watch and knows they have to spend another 45 minutes with the patient if they’re really going to make a difference.
So what do they do? They ask the patient if they’re having trouble sleeping, if they’re depressed? The patient answers yes, so they write a prescription. If you’re lucky, they’ll get onto the referral pad and send you to a psychologist who does have the time.
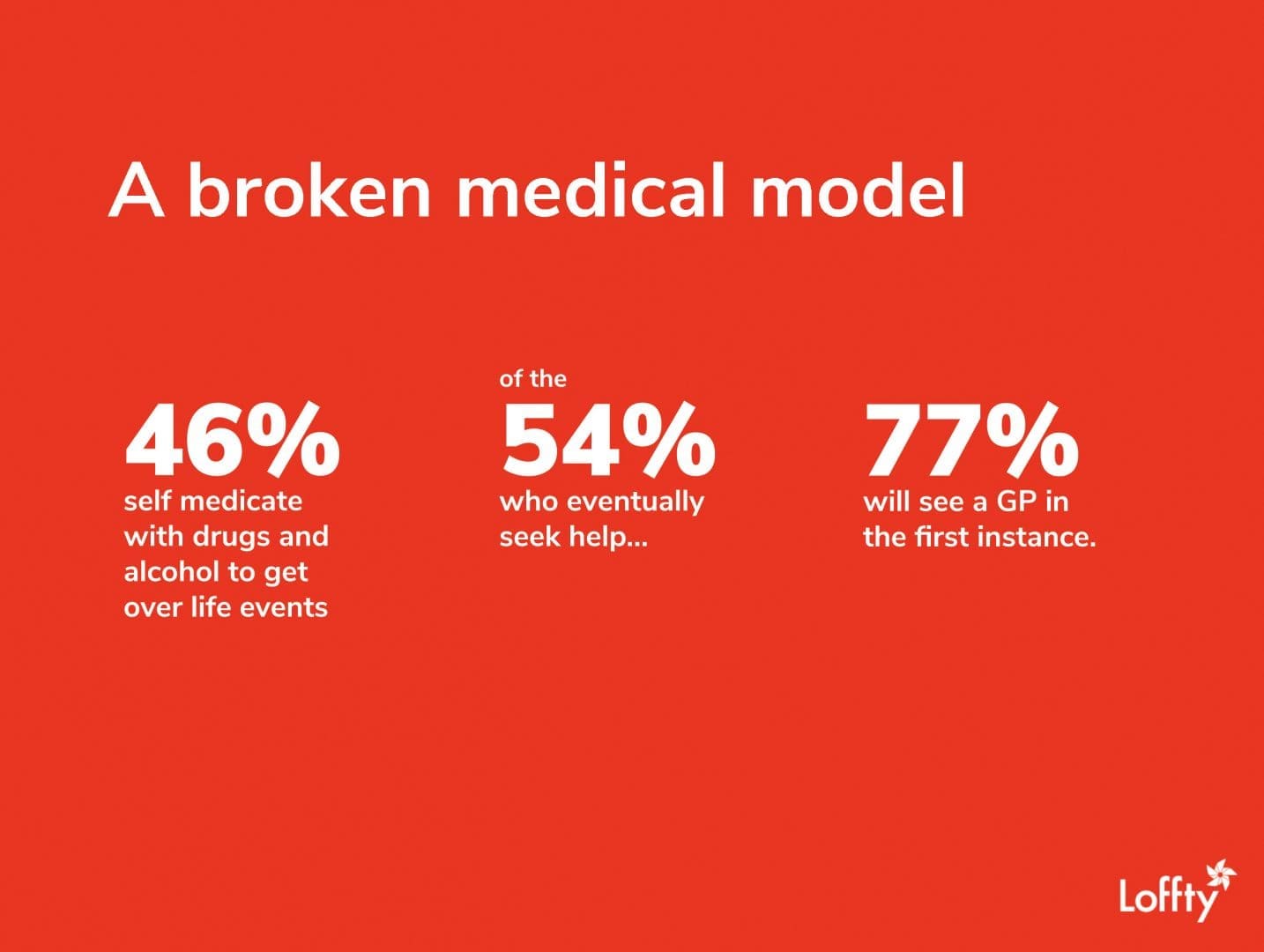
Things happen in life; marriage break ups, illness, death of a loved one. The world has sped up. Life has sped up and we’re just not coping. So what do most people do? 46% of people, when they have an issue or a challenge, they’ll turn to drugs and alcohol. They’ll binge drink on a Friday night because they got through the week.
We know from a recent US study that it takes on average 10 years for someone to get that help. Because of the stigma, they stay away, they don’t want to share their challenges. When you break your arm, you go to hospital in an hour. But with mental health, it’s different. Of the 54% of people who seek help, 77% will see a GP in the first instance. But as I’ve explained, this model is broken, they don’t have the time.
The deck is really stacked against the GP. They struggle with the fact that mental health is subjective. They’re trained in evidence-based medicine; blood tests, x-rays, CT scans. They don’t have a perspective on what they have to do for mental health in that timeframe.
How do we know this? We have the leading mental health assessment tool that’s been used by Australian GPs for the last 15 years. We know that this model’s broken because we’ve been a part of it for the last 15 years. It simply doesn’t work.

Here’s the problem with this model;
- Misdiagnoses: we know that more than half the people with a diagnosis of depression, that were referred by their GP to use our software, didn’t have depression, they had bipolar disorder. But in that time slot, the GP didn’t ask if they were ever manic. So what did they do? The gave them antidepressants. They’re giving antidepressants to a person who half the time is manic and needs to be brought down. The system is broken.
- Overprescription: There is such a massive over prescription of mental health medication, it’s not even funny. Don’t get me wrong, I’m not anti-medication. It’s being overused. There’s a time and a place for it, but not for mild or moderate issues.
- Missed diagnoses: There was a study out of Australia that looked at 47,000 consultations with GPs. In more than 50% of cases where there was a mental health issue present in those consultations, the doctor didn’t pick it up. For half the people who are being seen by a GP who have a mental health issue, it’s not even being discussed. This results in disappointed patients and patients lose hope. That word hope is really important around mental health, because it enables people to still strive to keep living. When patients lose hope, that’s when they self-harm and suicide.
When Jacinda Ardern announced the mental health review just after she was elected, she said if we want different results, we need to do things differently. So what did she do? She set up a six-person review panel with people from the mental health sector giving six perspectives and nothing new. There was representation on that panel for Pasifika, for Maori, for the Rainbow community, for the academic sector, for not-for-profit, for seniors. There’s not a problem with that. There was no one on the panel with any innovation, technology or business experience. There’s certainly something wrong there.
We have to ensure that we bring technology into this area as a solution. What did that panel do? The results came out in November, the government made its decision on how things will work: more of the same. ‘Let’s train more people, let’s throw more money at it, because it’ll look like we’re doing something, more than the other party.’ More of the same. It’s just perpetuating that myth that the medical model is able to fix this problem, but it’s not.
What are we going to do? What’s the paradigm change? Firstly, we’re moving away from a stigmatised, government-funded medical model to a technology-driven, innovative business model that involves businesses, the businesses of New Zealand. And when we combine this new business-led model of care with technology, with our platform, we can quantify mental health for the first time. For the first time, mental health will not be the poor cousin to physical health. We’ll be able to quantify it, and if you can quantify it, you can measure it. You can make business decisions for your people.
There are a lot of stats you can get from studies around the world. 11% higher revenue per employee when you’ve got well employees; 1.8 fewer days absence. You can measure all that stuff. These are studies that are academic studies, they’re a point in time. But they don’t provide actionable insights for you as business people. There’s a great Deloitte study recently out of the UK, that found for every $1 spent on wellbeing in your organisations, you get $4.20 back. That’s great, but where’s the actionable insight for my business?
That’s where we come in. We’ve got a SAS-based workplace mental health and wellness platform. It works very much like an employee engagement survey, as companies pay for your employees to access this platform. There are three major components to it. We’ve got this world-leading mental health assessment technology that we’ve had for the past 15 years.
We’re bringing that into the context of the workplace environment. It covers things like major depression, generalised anxiety disorder, postnatal depression, bipolar disorder, eating disorders, addictions, sleep, OCD, PTSD, ADHD, phobias. It’s comprehensive, in fact, it’s by far the most comprehensive assessment tool in the world.
We’re combining that with lofty insights. Your employees will use this assessment and they will get a whole bunch of insights for them, based on where they’re at at that time. And these are suggestions on what they can do to take responsibility to be empowered to look after their own mental health and wellbeing.
There are also business insights. So as a business, you will get de-identified, 100% confidential information about trends in your workplace relating to mental health and wellbeing.
For larger businesses, you will be able to tell that there are issues in this department, bullying happening in this department, too much stress happening in this department, this department is not fit enough; a whole bunch of information. In addition to those clinical mental health issues, we’re covering the big lifestyle issues; sleep, nutrition, exercise, social connectedness, purpose, personal financial situation, employee engagement. These are all things that contribute to the very complex space of mental health.
You’ve got your personal insights, you’ve got your corporate insights; what do you do with that? Your employees get lofty solutions, they get referred to a range of solution providers on our platform. These range from free reading and video material, to exercise platforms, to budgeting tools online, cognitive behaviour therapy, positive psychology, mindfulness, yoga, meditation, psychologists, career coaches, psychiatrists. Front end people that are face to face, and will be doing telephone help as well, to the materials people can get to educate themselves around mental health and wellbeing.
In addition to the personal solutions, where we recommend your employees to these things, there are solutions for the workplace. We’ll be working with workplaces to understand what they could be doing better for their people. Four day work week, remote working, job sharing; doing more than putting a fruit bowl in the staff room and having a once a year step program that 10% of the employees use, most of which would have been doing exercise anyway.
The difference with what we’re doing is that all of our solutions, your people will use them, you’ll use them and the data comes back, full loop. Our machine learning will be able to interrogate that data and become more accurate in its recommendations in the future.
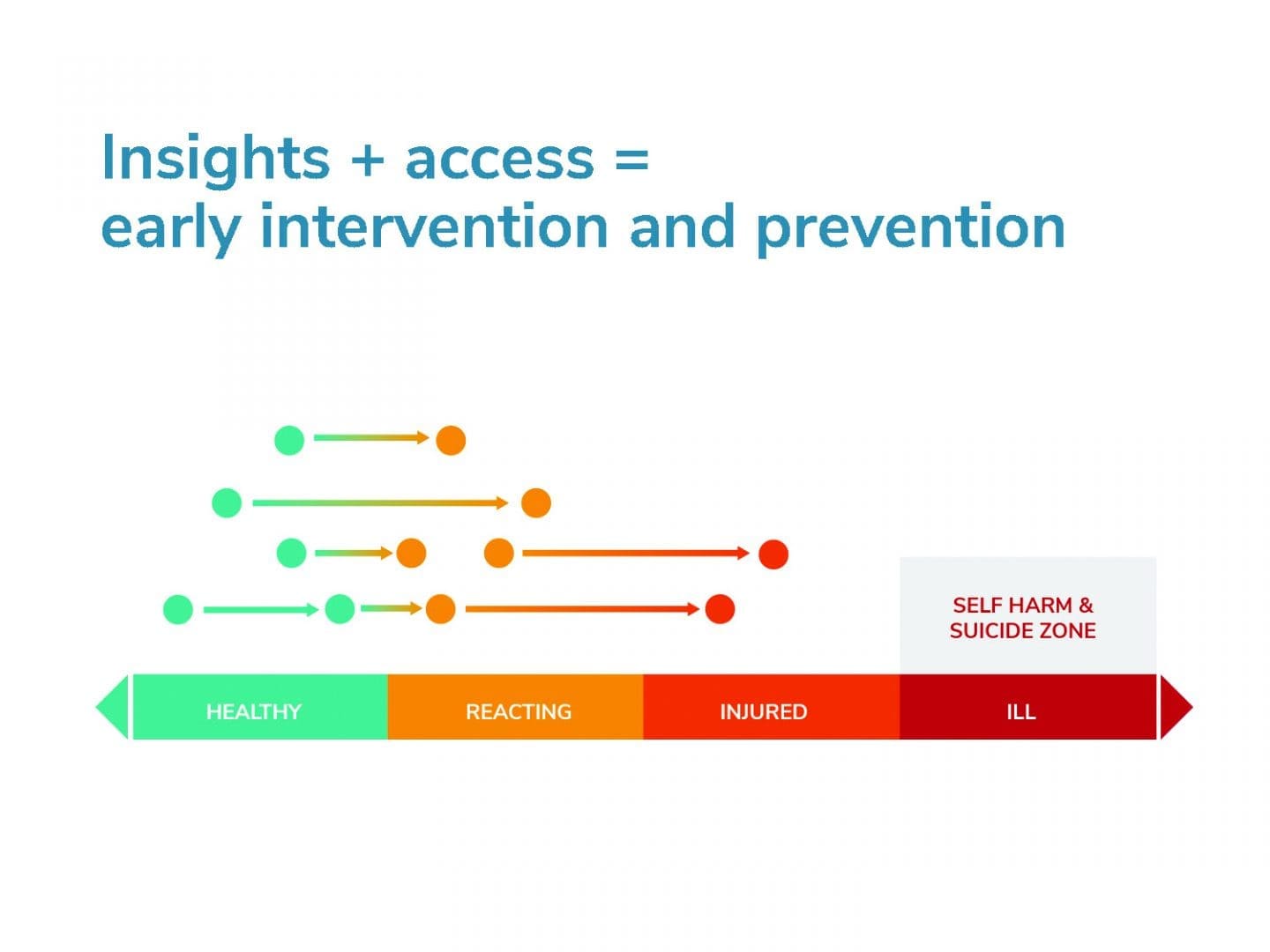
That brings us back to how this will make a difference to halfing the suicide rate in New Zealand by 2025. It’s all about early intervention and prevention. At the moment, EAPs (Employee Assistance Programmes] are late intervention. They get about 7% uptake rate within organisations, and people will only go and use those as a last resort. They hate it.
There is a time and a place for that, when people are really feeling ill and injured at that end. But so many of your people have life events that happen where they just need some support earlier, where they need some guidance, where they can use tools like sleep, exercise, nutrition and a range of other suggestions to look after themselves and be empowered to look after their mental health and wellbeing.
Events happen. 46% of people self-medicate, 10 years later, if they’re lucky, they’ll go and seek help about it. We’re getting in early. Our solutions cover the full range of people, but our solutions get people going back in the other direction so they don’t end up self-harming and suicide. This is where they lose hope. We need to prevent people from getting to that end of the continuum and if we do that, that’s how we half the suicide rate in New Zealand.
So together, using this business-focused, technology-led, innovative approach to wellbeing, we want you to join us.
Dominic Bowden: The hardest thing is vulnerability. What is a way to encourage the staff to be a bit more vulnerable?
Have a look at someone like Craig Hudson at Xero. Xero is doing amazing work in this space and their even going beyond that by offering to 6,000 of their customers access to their programme. The reason it’s amazing is that Craig is a leader. When you’re dealing with the workplace mental health and wellbeing of your people, it’s so much more valuable if you speak up as a leader, than if the staff are raising these things.
That vulnerability that he showed last year when he came out with his challenges, was incredible and it’s just done so much for Xero. There are people at Spark that are doing a great job as well. There are a lot of companies that are unfortunately just doing the same old, same old with EAP, but if you can take this on as a leader in your organisation, things will change and it will make a big difference.
Work is so much more than 9-5 and if you want to protect someone’s mental health and we need to focus on the rest of someone’s life outside of the workplace. Would you agree?
Completely. We spend roughly a third of our lives at work. If you’re not enjoying your work and the passion is gone, move on to something else. But do that with guidance, do that with love, do that with people around you will help you make those decisions. You spend a lot of time at work.
We interviewed a whole lot of large corporates in New Zealand and asked them what they were doing and what their biggest problems were. And their frustrations were when they had a really good staff member who one day just one decided they had to leave, they were burnt out. The World Health Organisation, only last month, has reclassified burnout as a workplace condition. So it’s a huge problem. If employers can identify these issues early, they’ll prevent some of their good people leaving without the employer having any idea that they were having challenges.

